Physicians and Engineers Use 3D Printing and Modeling to Determine Which Surgical Approach is Best in Aortic Valve Replacements
![]() We’ve seen 3D printed heart valve models used for training purposes before, as well as 3D printed patient-specific heart valve models and aortas used in pre-surgical planning. The latter is what physicians from The Ohio State University Wexner Medical Center and biomedical engineers from the university’s College of Engineering are focusing on – using 3D printing and personalized modeling to improve care for patients who need aortic valve replacements.
We’ve seen 3D printed heart valve models used for training purposes before, as well as 3D printed patient-specific heart valve models and aortas used in pre-surgical planning. The latter is what physicians from The Ohio State University Wexner Medical Center and biomedical engineers from the university’s College of Engineering are focusing on – using 3D printing and personalized modeling to improve care for patients who need aortic valve replacements.
“Having clinical and biomedical engineering faculty at the same table discussing individual patients makes our heart program stronger, and there are real-life examples of patient benefit. In some cases, for example, the coronary arteries come adjacent to where the valve would be placed. Using 3D modeling we can determine whether or not to protect these blood vessels during deployment, or even whether to proceed with valve replacement at all,” explained Dr. Scott Lilly, interventional cardiologist and co-director of the structural heart program at Ohio State Ross Heart Hospital. “These discussions have directly informed how we approach many valve replacement procedures.”

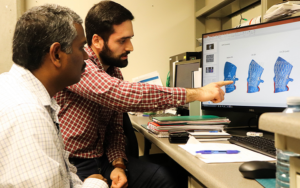
Dr. Scott Lilly reviews a scan of a patient’s heart at The Ohio State University Wexner Medical Center.
When a person is in need of an aortic valve replacement, typically it’s due to a narrowing of the valve opening called aortic stenosis. The leaflets of the valve can calcify and become stiff over the years, making it more difficult to pump blood from the left ventricle into the aorta.

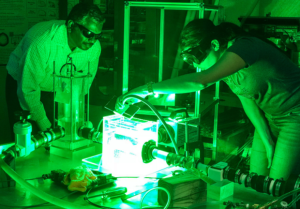
Dr. Scott Lilly performs transcatheter aortic valve replacement at The Ohio State University Wexner Medical Center.
Open heart surgery is one way of replacing a valve, but the less invasive method is transcatheter valve replacement, which sends in a tissue valve through one of the blood vessels in a person’s leg.
The OSU engineers and physicians are working together to help surgeons decide which approach and valve is right for each patient by developing patient-specific 3D models of the aortic valve and its nearby structures. This helps them simulate how the valve will function, as well as predict any potential complications.
“For most patients, available valves work comparably. However, in some cases the anatomy of the patient may create additional considerations,” Dr. Lilly said. “For example, the patient may have calcified nodules on the valve leaflets, or coronary arteries that arise in close proximity to the valve. The ability to reconstruct the areas where the valve is going to rest is important.”
Every week, Dr. Lilly and his structural heart team meet with Lakshmi Prasad Dasi, Associate Professor of Biomedical Engineering and Surgery at the university’s Davis Heart and Lung Research Institute. Dasi’s team then works to accurately reconstruct and 3D print the aorta of that week’s patient, using their CT scan and flexible materials.
The 3D printed model is then placed into a heart simulator, which will test the replica by pumping simulated, transparent blood through the system.
- Lakshmi Prasad Dasi, PhD, reviews a computer model of a patient’s heart with a graduate student.
- Lakshmi Prasad Dasi, PhD, tests a 3D printed aorta in a simulator.
Dasi explained, “Using laser and high-speed camera, we can measure blood flow velocity and vortex patterns with and without a replacement valve. We can model various therapies, positions and types of valves to better understand problems such as leakage, clotting or coronary obstruction. We can observe how different valves not only relieve the stenosis but also minimize the likelihood of blood clots forming on the leaflets, which is the goal of the treatment.”
Dasi’s team also makes computer models, in order to get a better look at the interaction between the transcatheter valve and the patient’s anatomy, along with the physics of blood flow.
This week, Dasi and Dr. Lilly presented their work at the annual CRT conference. The modeling work is funded by the Davis Heart and Lung Research Institute and the university’s TriFit Challenge Discovery Fund, and the long-term goal is to speed up the process of personalized treatment decisions by eventually being able to understand each patient’s unique blood flow and anatomy without having to use 3D printed models.
“We currently have two valves to choose from in the transcatheter world. I suspect we will have at least four within two years. Each valve is a little different, and the anatomy of every patient is unique,” said Dr. Lilly. “The ability to predict the function of the valve after placement, and which valve may work best with the least amount of leak and without impinging on adjacent structures, is critical. We are making progress.”

3D modeling of Bernice Belcher’s heart structure guided doctors at The Ohio State University Wexner Medical Center to perform open heart surgery to replace her aortic valve, rather than using a transcatheter method.
The 3D modeling work by Dasi and his team recently led doctors to choose open heart surgery for 78-year-old patient Bernice Belcher, instead of a transcatheter procedure. The Columbus resident was in need of an artificial valve, but 3D modeling was able to show the doctors that her aortic root was not long enough for them to use a transcatheter valve.
“The surgery was a great success. I didn’t have any chest pain,” Belcher said. “It’s astounding how I recovered from all this, and now I can get up, and I just have that ‘go power’ now.”
With funding from the National Institutes of Health (NIH) and the National Heart, Lung, and Blood Institute, Dasi’s team is also working to improve the bioprosthetic valves by developing novel synthetic heart valves that are enhanced with biomolecules, making for more cost-effective and durable transcatheter valves.
“Young patients who need an artificial heart valve often get a mechanical version, which requires taking blood thinners for life. It’s our hope to develop a more durable valve with superior blood compatibility, and possibly eliminate the need for blood thinners in these patients,” Dasi said.
Discuss this and other 3D printing topics at 3DPrintBoard.com or share your thoughts below.
[Source: The Ohio State University / Images: OSU’s Wexner Medical Center]
Subscribe to Our Email Newsletter
Stay up-to-date on all the latest news from the 3D printing industry and receive information and offers from third party vendors.
You May Also Like
Nylon 3D Printed Parts Made More Functional with Coatings & Colors
Parts 3D printed from polyamide (PA, Nylon) 12 using powder bed fusion (PBF) are a mainstay in the additive manufacturing (AM) industry. While post-finishing processes have improved the porosity of...
3DPOD Episode 193: Flow and What’s Possible in 3D Printing with Ricky Wildman, University of Nottingham
Ricky Wildman is working on 3D printing pills, but, as Professor of Multiphase Flow and Physics at Nottingham, he does a whole lot more. His research encompasses the characterization of...
3D Printing Webinar and Event Roundup: March 17, 2024
It’s another busy week of webinars and events, including SALMED 2024 and AM Forum in Berlin. Stratasys continues its in-person training and is offering two webinars, ASTM is holding a...
3D Printed Micro Antenna is 15% Smaller and 6X Lighter
Horizon Microtechnologies has achieved success in creating a high-frequency D-Band horn antenna through micro 3D printing. However, this achievement did not rely solely on 3D printing; it involved a combination...